[00:00:00] Speaker A: Foreign.
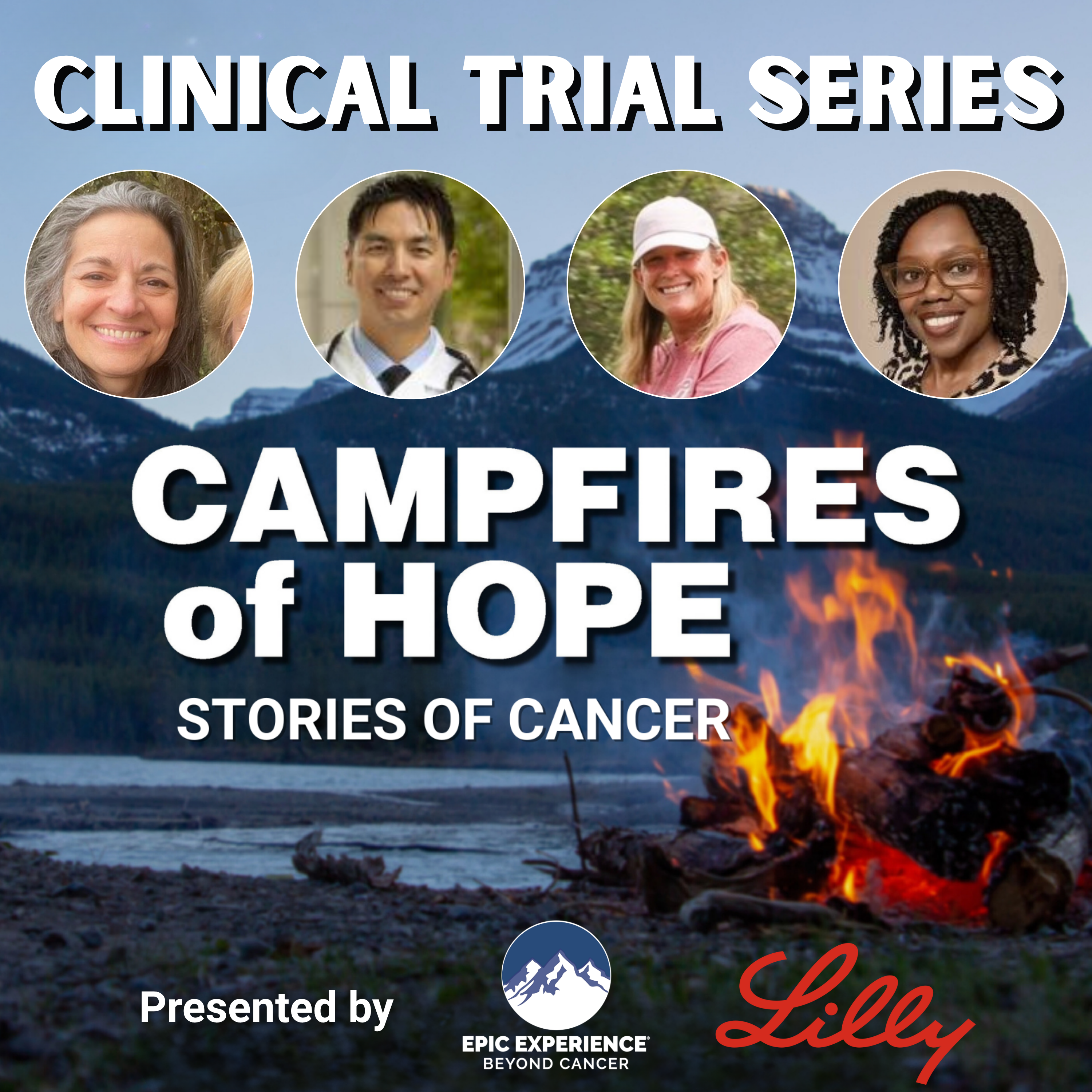
[00:00:08] Speaker B: My name is Nancy Farrow, also known as Mama Lu, and I'm the founder of Epic Experience.
Epic Experience mission is to empower adult cancer survivors and thrivers to live beyond cancer.
I hope that as you listen to campfires of Hope living beyond cancer, you find hope, healing and empowerment.
Through stories and education, we aim to guide those impacted by cancer and more importantly, offer love and support to anyone out there who needs it.
This is beyond Cancer.
[00:01:13] Speaker C: Hello everyone, this is Gail, AKA Sunshine. Today I have Lori Downing joining us around the campfire.
January is Cervical Cancer Awareness Month and we're honored to have Lori join us and share her story and perspective as a cervical cancer survivor. So, Lori, we welcome and thank you so much for joining us.
[00:01:33] Speaker A: Thank you so much, Gail.
I'm very honored to be a part of this and a little nervous, but I'll just do the best that I can.
[00:01:41] Speaker C: You're going to do great. But why don't you just start by telling us a little bit about yourself, where you're from, your family, your career and that kind of stuff. And I always ask people to include one fun fact. Okay.
[00:01:52] Speaker A: I'm, I live in, in Nassau County, Long Island. I was born in Queens.
My family moved to Suffolk, out to Suffolk County, Long Island. And I met my husband, upstate New York College. He's a Staten Islander, so he's a New Yorker too. And then we moved, we had a family and we moved to Nassau county where we still live.
I have 37 year old son, a 32 year old daughter.
I'm retired about five or years ago, in 2020, I guess six years ago as a teacher.
I taught for about 35 years and I really enjoy retirement and I travel a lot. And I would say the fun fact about myself is that I go on a lot of yoga retreats and I've traveled several times on retreats to Costa Rica, Greece, Spain, Ireland, Sicily.
The next one I'm going to is Portugal at the end of the summer and I started going solo or with groups and my husband, I guess about two years ago was like, because he doesn't practice yoga or meditation or mindfulness. And a couple of years ago he's like, I want to go on some of these trips too. So he started coming with me. Oh yes.
[00:03:25] Speaker C: Oh, that's great.
Well, the thing that brings us to here together today, obviously is cancer and specifically cervical cancer. So I'm wondering if you can tell us a little bit about your diagnosis story, when you were diagnosed, how you found out, you know, quick synopsis of your treatment and all that.
[00:03:43] Speaker A: Yeah. So it was the summer, June, July, of 2013, and I went for my annual Papa, and I was actually camping. This big thing I do. I camp out on the beach in Montauk a lot. And I was camping, and I was in the car with a friend, and my GYN actually called and said, are you by yourself? And I'm like, well, no, I'm with people driving in the car. He goes, I hate to give this news over the phone, but you have cancer.
He says, it's going to be okay because it's early and you're just going to have. I set up an appointment for you, and it'll just be a lapras Scope.
Long story short is I decided.
I researched a little bit, and because I live so close to the city, I said I might as well go to Memorial Sloan Kettering Cancer Center. I have access to a premier cancer center.
So I made an appointment there, and I had a surgeon that she chose to do a radical abdominal hysterectomy. That's a little bit more invasive, you know, I guess. And. And in a radical abdominal hysterectomy, they kind of take out just about, like, everything. Your uterus, your cervix. Yeah.
Your. A lot of ligaments and muscle, you know, around. And the top third of your vagina. And I. When she told me that, I was like, no, no. I go, I don't want that done. She goes, you have no choice. You're having that done. You know, for your. What you have. You're at later stage of stage when you have to have that done. I remember saying to her, this kind of gets to the sexual part. Remember saying to her, how is, like, you know, a penis. My husband's penis going to fit? And she said, oh, the vagina is very elastic. It's very stretchable. And she just kind of dismissed it. That was that. And I made the appointments very quickly. I was in the city at Sloan for about one week.
Aside from physically recovering from abdominal surgery, that was the only physical part. And I mentally. I did very well at the time, and I was very lucky that I did. Nothing was found in my lymph nodes, and I did not have to have any radiation because radiation with cervical cancer is all internal. It's. Yeah.
[00:06:12] Speaker C: Oh, yeah, yeah.
[00:06:13] Speaker A: It sounds pretty brutal. And I didn't have to have any chemo, and I've had.
[00:06:17] Speaker C: Oh, wow.
[00:06:18] Speaker A: I've been. No evidence of disease for the past 11 years.
[00:06:23] Speaker C: That's wonderful. So every. I mean, not that surgery was easy. And I'm Sure. There have been changes, which we're going to talk. Talk about, but you didn't have to do any treatment, which is wonderful, right?
[00:06:32] Speaker A: Which is just, you know, you know, surveillance. You know, it was in the beginning, I had to go every three months and every six months. And then after five years, she. She caught me loose. She says, no. She goes, you go to your regular GYN now.
[00:06:46] Speaker C: Wow, that's. Congratulations. That's wonderful.
[00:06:48] Speaker A: Thank you.
[00:06:49] Speaker C: So for you, what physical, mental, emotional challenges stand out for you both right at that time? And even as time has progressed.
[00:07:04] Speaker A: I'm gonna get a little emotional because when I think about it back, looking back on it, because at the time, Gail, I was very.
I had to be very strong. And I did not. I kind of didn't want anyone to know. I didn't want my husband to get upset. I didn't want my kids, you know, they were, you know, they were. It was like say 10 years ago, so they were a bit younger, not children, but, you know, they were adults, but younger.
[00:07:35] Speaker C: They were in their twenties. But still they're your kids.
[00:07:37] Speaker A: Yes.
And I just didn't want to. I knew I was nervous enough myself and I didn't want to deal with other people's nervousness.
I did go. I went to all because there were some procedures and smaller procedures I had to have done beforehand. And I really did do everything myself. I did have one sister that came with me some things. I couldn't drive and she came with me, but I didn't even, like, use the word cancer to my husband and my kids until the night before I had the surgery.
And that was. And the reason was, was because I went right before to my oncologist, the surgeon in the city, and she was very matter of fact. She was wonderful. Very matter of fact. And she said something to me about your children, your husband. Oh, I know my husband was going to be there. I said, oh, just. I want to Let you know, Dr. Brown, that when you, you know, in surgery, whatever you find, do not tell my husband. You go, I want to know. Wait until. Tell me first and I will tell him. And she looked at me and she said, does he know? And I said, no. And she said, I don't. I'm not going to do the surgery. I don't think you're ready. And I was like, oh, I'll tell him. You know, I will tell him. So that night we went out to dinner with my husband and my son and daughter. And I told them and I tried to. Well, you know, it is really it is cancer, you know, But I think they kind of went over their head a little bit because I was a little nonchalant about it. And when I look back on it now, I was like, I don't know why.
I think I probably should have relied on people a little bit more, you know, I don't know, like, why I had to. Felt like I had to protect people.
[00:09:37] Speaker C: Yeah, I think it's. You're not the first person to tell me that. I have heard that number of times, and I experienced it myself. I think it's just a natural thing. We're dealing with our own shock, fear, pain, you know, whatever.
[00:09:50] Speaker A: Yes.
[00:09:51] Speaker C: And to add, the. The additional shock, pain, fear of others can seem like a little too much, so I can understand that.
So what kind of. What did that do to your relationship with your kids and your husband? Did it impact it once they realized what we were really dealing with?
[00:10:14] Speaker B: I.
[00:10:14] Speaker A: You know, that's an interesting question. I don't know.
You know, I did see, you know, my son. My daughter got. Was kind of became upset, which I didn't want. I didn't want to have to deal with her being upset and trying to console her and try to make her better. Where my son became very protective. My husband more like my daughter not crying, not, you know, like that. But I could tell he got worried, internalized it, worried. Where my son became more like the protective, practical one, you know, And.
And, you know, it probably, you know, strengthened my relationship with all three of them.
[00:10:56] Speaker C: It really did, I'm sure. I mean, it's interesting how each family goes through it, and that's interesting that that was the final outcome, which is great.
[00:11:04] Speaker A: Yeah.
Just very funny. My son, that was just here that I made leave. We are very close. But there was one thing, maybe it was like a couple of years later. I, you know, a lot of times I want him to do things he doesn't do. And I never. This is. I only. I was so desperate for him. I can't remember what it was. Something silly. I was so desperate for him to attend whatever I wanted to him to attend or go. And I was like, you have to do it. You know, I had cancer and he looked at me and he said, oh, no. He goes, you can't use that card ever.
[00:11:39] Speaker C: That's neat. Well, that says something about your relationship. That is pretty funny. Thank you for sharing that. I love it.
So if you think about your experience, specifically given that you had cervical cancer, what challenges did you face as a gynecological. Gynecological Oncologist.
[00:11:58] Speaker A: Patient.
[00:11:59] Speaker C: That's the hardest word to say, both from the point of accessing information about, you know, sexual health and navigating the stigma around having cervical cancer.
[00:12:10] Speaker A: Yeah. Well, just. Okay, let me first tell you the stigma part. Sure. That was something. When I was first initially diagnosed, I was like, oh, my gosh.
Because, again, it was only 11 years ago, but I. Maybe because I'm more educated and also because I think a lot has changed in the 11 years, too.
Yeah. I was a little embarrassed, you know, at first, and I was like, you know, and I actually said to my husband, because I. We met in college, you know, he was not my only sexual partner, but very, very few compared to him. And I don't want to make it sound like he was sleeping all over, but. Difference between men and women. Yeah. You know, and so I kind of said, you know, it was. It has to have been from you, you know, that I got, you know, and he was like, really upset that I said that because, well, that's not fair, you know, and really, in reality, because of, you know, the way it goes, it could be anyone. And you, you. I could have.
I could have had one other partner besides him. And. But that.
I can't, you know, how to explain it. It just. It just passes so, so easily. So it really, really has nothing to do, like, with sex. It doesn't.
[00:13:29] Speaker C: Well, that's what I was going to say. I mean, it's cervical cancer. And yes, there's the HPV virus. Right. I mean, that's.
[00:13:35] Speaker B: Yes.
[00:13:36] Speaker C: But at the same time, it's cancer, which. Cancer's not transmittable in the same way that, you know, having the flu is or something?
[00:13:45] Speaker A: Yeah. Yeah.
[00:13:46] Speaker C: So would you say that's why you had. You had that stigma, that shame was absolutely. It was connected with sexually transmitted 100.
Yes, that is completely understandable.
So in terms of accessing information about sexual health, how did. How was that?
[00:14:05] Speaker A: Okay, so again, going back into 2013, when I realized, you know, she had initially told me, oh, don't worry, you're not going to have any problem. Because it's not like, usually the women, the internal radiation, I think it's. I don't know if I'm pronouncing it correctly. It's called bracket brachytherapy. Brachytherap. Brachy. You know, those. You're. You're having your inside of your vagina burnt, you know, so those women are like, they have very lot. Very difficult with sexual activity or intercourse. And so she says, well, you don't have that but then when I was seeing I was having difficulty or pain, and I tried talking to her about it was a little disappointing. You think, here I am at a premier cancer center and this doctor is not caring about that part of my journey.
And then she, I think, finally sent me. They did have a sexual health wellness part of Sloan. And I did go to that doctor. And you know, again, they were all like, very nice, but I don't really think they gave me very good tools. Finally, I would say a few years later, me just like, pressing it, pressing it. They. And again, maybe they didn't even have these departments open yet. Maybe they were opening. As time went by, I did go to a pelvic floor therapist. And that was a really interesting thing. I was like, oh, how am I going to do this? And it was like, so bizarre because you go. And it's. I don't know if any. Anyone who's been part of pelvic floor therapy, but you're really having.
And of course, I think women. I think it's usually women working with women. These two wonderful young girls. You know, you're having these huge.
Oh, God, I can't think of the word. The, the plastic.
Oh, my goodness. This. I really should.
Yeah, well, I didn't want to say dildo. This is a more professional.
[00:16:13] Speaker C: I'm sure there is. I don't know what it is, but there you go.
[00:16:16] Speaker A: I should know it. I should know it. And, you know, so they give you all different, varying. And so you're in with the first. They're putting their hand up you there, because then there's a little scar tissue, you know, and they're, you know, they're. They're moving it around and then you're doing it and you're. So. It's really. But you. Oh, my goodness. The relationship you form with these people.
[00:16:37] Speaker C: I would imagine so it's interesting. That's not what I thought you were going to describe it as. I was thinking of more strengthening, which I'm sure that's part of it, but it's learning how to do this again and, and using the muscles in the way.
[00:16:53] Speaker A: Yeah, using the most interesting. I mean, yeah, it's like you could do like the, The Kegel, like, type muscles. And actually they. That's how I probably got into yoga. You know, they recommended yoga because that does. That's a lot of pelvic floor strength.
And. And then the. The yoga became a whole thing for, you know, meditation and mindfulness. So it, it helped me mentally, too.
But. Yeah, but that was the kind of little bit disappointing thing that I felt as though I was not really given support for the sexual health aspect.
[00:17:29] Speaker C: Yeah.
I don't think you're alone. And I'm sorry that was your experience, but I'm glad that you ultimately got what you needed. Yes, that sounds like a bonding. Definitely a bonding experience.
[00:17:44] Speaker A: And also to go back to using dilators. That's the word, dilators.
[00:17:50] Speaker C: That's much better.
[00:17:51] Speaker A: My word using it was a D word. Using the dilators is that it can, you know, you have to practice it then at home at night and it can become a chore, you know. And with. When I speak about Survivor, the organization I do know too, speaking to those women there, you can, you know, with your partner, you can make it into games or that Lana. That I'm just maybe just not open enough for that, you know. Yeah, so. Yeah, interesting.
[00:18:25] Speaker C: Yeah, that is. That's a whole part because of the kind of cancer it is that other people don't. Lung cancer. You're not going to have, you know. No, it's just a unique aspect for sure.
[00:18:35] Speaker A: And Gail, sometimes I feel very guilty about speaking about it so much because it's like, yeah, you had. I had cancer and I completely survived it. So to be complaining about this is when you see other people dealing long term and with reoccurrences, you know, it sounds a little whiny to be.
[00:18:55] Speaker C: And yet.
Yeah, and yeah, no, I understand that, but. And yet it is your experience and you have had to relearn. I mean, it impacted you long term, which is one of the things we talk about with epic experiences.
When your cancer journey is over, it's not really over because there's all these other side effects that can be long term, mental, emotional and physical. Obviously in your case too, are there. You reference this kind of tangentially, but the cervical cancer groups and networks are there ones that you have been part of that you would recommend?
[00:19:29] Speaker A: Yes, there is this and I didn't know about them originally and again I. They were. Is called survivor.org and I kind of have wrote it on this little paper and I don't know if like you or Chris somehow will maybe be able to pull the website up, but they're an amazing group and Tamika Felder is the founder and she was diagnosed in her 20s with cervical cancer. And I met a lot of women, A lot of women. Do you think that it's older, but there's a lot of young women that get diagnosed and sadly for a lot of them, they lose their Fertility. Sometimes they can have fertility sparing surgery, but some of them have lost their fertility. But this group has just gotten celebrated 21 years.
So professional and so knowledgeable, and what they offer is incredible. So that's just. I just want to tell anyone to please check out their website. They have a Facebook page that's amazing.
I have it written down here a little bit because it's a nonprofit organization dedicated to raising the awareness about cervical cancer, supporting survivors through education, advocacy and community.
They're really, really big on survivors. I haven't done this yet, sharing their stories like little clips, because then you get to see the whole range of what stage and what your treatment is and what you've gone through.
They also do. They just had one in D.C. that just ended last weekend. Once a year they do a cervical cancer summit for. Usually for a weekend.
And once a year they do. It's called survivor school that you could. Similar to like, epic you can go to once, you know, and. And you become a survivor ambassador. And a lot of I do have gone to their summit. I've never done their school because you really have to make a commitment to them when you become an ambassador. And I've gone to a few of their things where actually last winter I went into the city.
They had their. There's a group of surgeons, cancer surgeons that are also musicians. And we went there and we gave up survivor information and the pens and the pencils and things like that. So they're really big into advocacy and education, and it's a big commitment, you know.
[00:22:17] Speaker D: That's great.
[00:22:18] Speaker C: Wow, that sounds like a wonderful resource. Thank you for sharing that.
What do you think the biggest lesson you've learned throughout this cancer journey? So for you, it's been 12, 13?
[00:22:29] Speaker A: Yeah, about 11. I think it's about 11 years. Yeah.
[00:22:33] Speaker B: I think.
[00:22:33] Speaker C: What do you think the big. And I know this is going to probably be hard to narrow it down, so feel free to give me a couple lessons. But what do you think the biggest thing you've learned is over this journey?
[00:22:42] Speaker A: You know, I kind of like wrote it. The first one that comes into my mind that I don't have to look at is, oh, that you're. You're stronger than you think you are. Yeah, you know that that's like the biggest lesson. And.
And.
And also.
Yeah, you're really.
This is kind of cliche, but, like, you're never too old to learn something new or experience. And that was. I kind of tied that into like the epic, the camp that. That was something that I Could do a whole podcast on that, that story, the anxiety I had about going there, but that was like something that, you know, I can't do this, I can't do this. And I learned that helped me realize that you can always stretch yourself out of your comfort zone, you know, always.
So.
[00:23:28] Speaker C: So for you, it was going. The thinking about going to Epic was anxiety producing. I'm curious why.
[00:23:35] Speaker A: Yes, because I started looking at their videos and like, and. And to see I' a little bit, like, afraid of water. Not silly. I'm a beach person. But I can, you know, I can bob in the water, I can go in the ocean, but I'm not like a long distance swimmer. I'm not an underwater person. And so when I started seeing the videos and this was like back in the day where you were just like in the kayak by yourself.
[00:24:00] Speaker C: Yeah.
[00:24:00] Speaker A: And you're doing like these like, rapids and. Oh, then I showed on the video when they put you in the pool and they put you upside down, like, that was like. I was. I have a fear of drowning, you know, And I was looking at that and I was like, like, I can't do this. I go, why am I doing this? This does not look like fun at all. Why would I put myself through this?
[00:24:21] Speaker C: So what got you to go? That's. That's my next question is what got me to go?
[00:24:25] Speaker A: I went only because I, I forced myself.
[00:24:30] Speaker C: Okay.
[00:24:31] Speaker A: I did for. Because I knew. I knew in the end if I didn't do it, oh, I have a lot of FOMO fear of missing out.
So I was like, if I didn't do this, I would probably regret it.
[00:24:42] Speaker C: Yeah.
[00:24:43] Speaker A: But I didn't do it.
[00:24:44] Speaker C: What would you say is the best thing that came out of it? So you forced yourself to go.
Are you glad you went? I guess.
[00:24:52] Speaker A: Yes. Oh, amazing. Amazing.
[00:24:54] Speaker C: So what is the best thing for you that came out of it?
[00:24:58] Speaker A: You know, that, that, that sense. Sense of strength and the sense of.
I would have to say, you know, the.
I mean, like I've said again, the people that I met there, you know, it's.
And even though, like, we're not in contact because the closest people, because there were like five of us that met and the air and at the Denver airport because other people were maybe in the area and the, the people that I traveled with to and from, unfortunately, Volt passed away and. Yeah. And so.
And so over these years, you know, that I've.
I guess it's probably close to 10 years, you know, that I've seen just the Last person. It was like, in my mind, I was like, okay, did it.
[00:25:58] Speaker C: He.
[00:25:58] Speaker A: Tom died. And I go, so you know who's alive? I go, no, no, alive. And then I got the notification that he died, and I was like, okay. And it's. You know what? It's very impactful to me because they were in my lives, and.
And it's. I don't really talk about them with anyone, and.
But they'll always, like, be a part of me. And sometimes I think, oh, when I do my manifest, my mindfulness or my mant.
[00:26:34] Speaker C: Like.
[00:26:35] Speaker A: Like fortunate or I am blessed. And I almost feel as though I don't want to say that I am blessed or I'm lucky compared to them, because I'm not any luckier than they are. They. They were.
They were just such amazing people that they probably have. They might have lived better. And I don't. I don't mean to say it like that they might have lived a better life than I did or what their life was. Was wonderful. Yes. And so I.
I feel as though I have abundance. I've changed that into.
Instead of being like, I'm fortunate, I'm grateful that. That I have abundance, and they're part of that abundance.
So I feel like it. Yeah. That I'm not. I'm not lucky compared to them. I don't know why it's. It's important for me to think of it that way.
[00:27:30] Speaker D: Yeah.
[00:27:30] Speaker C: Well. And they will always be part of that abundance for you.
[00:27:33] Speaker A: Yes. I mean, that.
[00:27:35] Speaker C: That's the really cool part. Was there anything else you would want to share with someone Listening.
[00:27:43] Speaker A: I'm trying to think. I don't know. I don't know if I gave, like, the best advice. I think I just talked really just about myself, but.
[00:27:50] Speaker C: Well, no, anything. I mean, anything. It could be a lesson. It could be something for a caregiver. It could be. I'm just wondering if you have anything else I haven't specifically asked about that.
[00:27:58] Speaker D: You would want to share.
[00:28:01] Speaker A: You know? You know, Gail, you know, I don't know if I have, like, any such great words of advice, because I still see people that I know that have, like, cancer diagnosis and sometimes how, like, I approach them. I've tried to approach people like, oh, I went through this. You know, I can help you. And they don't want to hear it.
And then people that get, like, offended if you don't ask so much. So sometimes I don't really, like, have any advice for it. The only thing is, I can think of is, you know, I guess you have to be there for people and you really, really have to pay attention and to how they're reacting and, like, what they're saying and re. You know, react to it that way. I did. And. And share if you can. If. If they seem like they're willing and open to it, go for it, you know, like, take the risk, because I will. I'd rather take the risk and maybe like, offend, not. I don't know if offend is the right word or overstep with someone and possibly help them than not say anything for fear of offending them. Like, you know, for example, even when I was set up, I'm in the library when I. Speaking with a young woman, I said, I'm going to be doing this, like, you know, cancer podcast I've never done. I'm nervous that I'm a boomer. And she was coming down, she showed me this room, and she said, oh, you know, what kind of cancer? And I said, oh, cervical cancer. And she said, oh, you know, I'm a. She was young. She's like 35. She's. I'm a breast cancer survivor.
And she started sharing with me, you know, and I was like, I hope you know what you have to look into. You know, And I like, type like this epic. I go, you have to go to this. I go, I know you have two young kids and you're going to say, you know, can't do this, or you don't have that time. I go, but you have to do this. Please do it. So probably I'll see her. I will probably, like, a little bit say, did you. And she seemed a little receptive to it, but. So I would say not your offer. And then, yeah, you know, and then see how people react. But don't ever stop offering, I think.
[00:30:12] Speaker C: Yes. Well, and you said earlier, you referred to sharing your story, and it's the same kind of thing.
[00:30:18] Speaker A: It's.
[00:30:18] Speaker C: It's. It's your story to share. And you never know. Like, if you hadn't said what you were doing, you wouldn't have had the conversation with this woman. You just never know who you're going to impact by just sharing that little bit. So I think that's great that you did that. So the way I always end the podcast is to ask this very important question.
Marshmallows over a campfire, slow and steady or flaming crispy.
[00:30:42] Speaker A: Okay. Of course I've looked at that. I'm gonna say, I won't make it. Usually I make a big thing of it. I'LL have to say go with slow and ste.
[00:30:50] Speaker C: Slow and steady. I love it. Well, Lori, thank you so much. Thank you for being honest and open about all the things.
I really like what you said about removing the stigma because I think that's very important. If people are going to get checked and catch this early, that has to be taken away.
[00:31:09] Speaker A: Yeah. And actually, I'm sorry, I know if I didn't speak enough about that, I spoke too much about myself.
I guess this can be edited out if you don't need, if you don't want to use it. But the big thing about the HPV vaccine, when I was, as I said, I'm retired. But when I first was diagnosed and I was speaking to other teachers that had daughters younger about getting the vaccine, I heard, and I still hear a lot of women and I get angry about it because I find it very ignorant and say, oh, well, no, why should I do that to a 9 year old year old or 10? So they're not sexually active. It's so, so they are, they are talking about it being related to sex and you know, it shouldn't be, you know.
Yeah, yeah, yeah.
[00:31:59] Speaker D: No.
[00:32:00] Speaker C: Thank you for sharing that. I appreciate that.
All right, well, thank you so much for joining us. And for those of you who are listening, until the next time we gather around the campfire, keep Living Beyond Cancer.
[00:32:17] Speaker D: Thank you for listening to this episode of Campfires of Hope, Living Beyond Cancer. For more information about Epic Experience and our programs or to donate, please visit our
[email protected] Music for this podcast is provided by Moonshiner Collective. If you enjoyed this episode, please rate and review us so we can share our story with more people. Also, be sure to subscribe wherever you get podcasts so you'll know when new episodes are released. We hope you come back and join us for our next episode.
[00:32:59] Speaker C: We will rise once again.